What is personalized medicine?
Accelerating Discovery at The Jackson Laboratory
Learn more about how our scientists are accelerating discovery in order to find more effective, precise, and personalized ways to treat, prevent, and cure diseases like cancer.
What is precision or personalized medicine?
Would a teenage boy buy the same clothes as his grandmother? Probably not. But when they get sick, they’re likely to receive the same medical treatment, despite their many differences. And so will everyone else.
That’s because even the world’s best scientists and doctors don’t fully understand yet how different people develop disease and respond to treatments. The result is a "one-size-fits-all" approach to medicine that is based on broad population averages. This traditional practice often misses its mark because each person’s genetic makeup is slightly different from everyone else’s, often in very important ways that affect health.
The advent of precision medicine is moving us closer to more precise, predictable and powerful health care that is customized for the individual patient. Our growing understanding of genetics and genomics — and how they drive health, disease and drug responses in each person — is enabling doctors to provide better disease prevention, more accurate diagnoses, safer drug prescriptions and more effective treatments for the many diseases and conditions that diminish our health.
Tailoring health care to each person’s unique genetic makeup – that’s the promising idea behind precision medicine, also variously known as individualized medicine, personalized medicine or genomic medicine.
What are the benefits of precision medicine?
Throughout history, the practice of medicine has largely been reactive. Even today, we usually must wait until the onset of diseases and then try to treat or cure them. And because we don’t fully understand the genetic and environmental factors that cause major diseases such as cancer, Alzheimer’s and diabetes, our efforts to treat these diseases are often imprecise, unpredictable and ineffective.
The drugs and treatments we devise are tested on broad populations and are prescribed using statistical averages. Consequently, they work for some patients but not for many others, due to genetic differences among the population. On average, any given prescription drug now on the market only works for half of those who take it.
Personalized medicine, because it is based on each patient’s unique genetic makeup, is beginning to overcome the limitations of traditional medicine. Increasingly it is allowing health care providers to:
- shift the emphasis in medicine from reaction to prevention
- predict susceptibility to disease
- improve disease detection
- preempt disease progression
- customize disease-prevention strategies
- prescribe more effective drugs
- avoid prescribing drugs with predictable side effects
- reduce the time, cost, and failure rate of pharmaceutical clinical trials
- eliminate trial-and-error inefficiencies that inflate health care costs and undermine patient care.
How is JAX connecting genetics to medical practice?
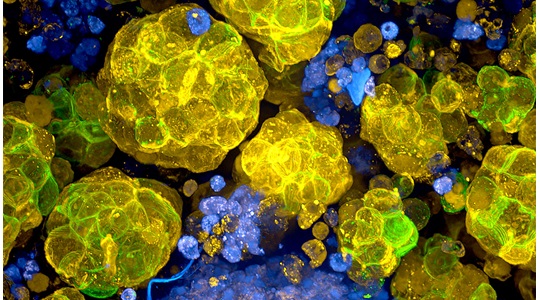
The interactions among hundreds of genes and gene networks, along with external factors such as diet and exercise, determine our biological traits — hair color or cholesterol levels, for example — and our health status. Systems genetics is a comprehensive approach to studying and understanding this biological complexity.
Mining vast databases with powerful statistical tools, geneticists, mathematicians, physicists and computer scientists are generating new insights into how genetic complexity drives health and disease.
The Jackson Laboratory has deep expertise in systems genetics that gives us a distinctive edge in the quest to understand disease. This capacity also brings us closer to personalized medicine that’s targeted to each individual’s unique genetic composition.
Our research helped explain why some patients did not respond as expected to Gleevec, an effective drug for some forms of leukemia. It also identified an additional drug that can be used with Gleevec to potentially help these patients.
Our systems genetics group is mapping the dozens of genetic interactions that give rise to type 1 diabetes. Others are deciphering the gene network that controls levels of HDL, the "good" cholesterol, in our blood. And researchers in our Aging Center are untangling the web of genetic and environmental factors that make us grow old.
We also house and maintain the Mouse Genome Informatics database, the world’s most comprehensive collection of mouse genetic data. This global resource is essential to understanding genetic complexity not only in mice, but in humans, who are 95-98% genetically similar to mice.