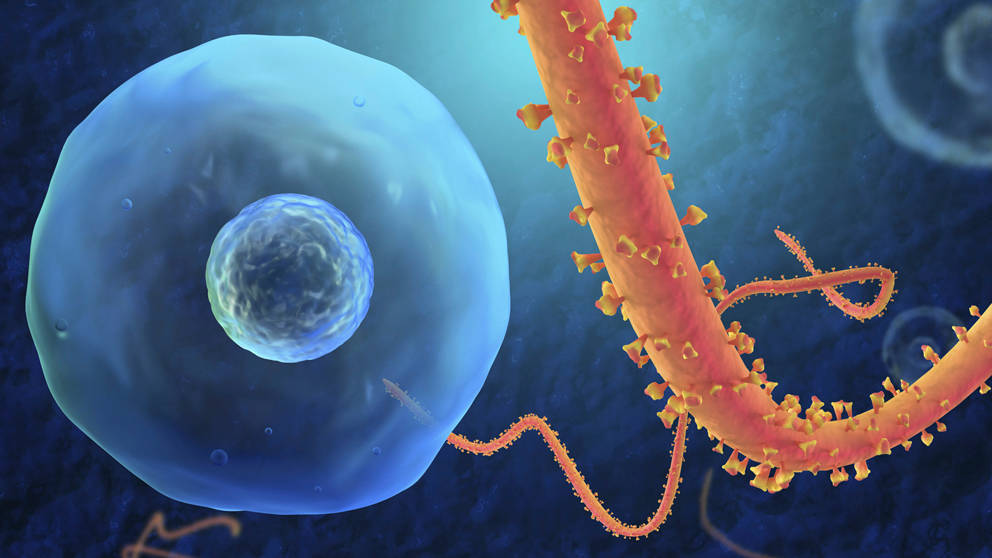
Thousands of people have been infected by the Ebola virus in West Africa in the recent outbreak. In response, the United Nations and the World Health Organization have implemented critical initiatives and are devoting over $56 million to halt the spread of the disease and address the social and economic consequences of the outbreak.
 The devastating mortality rate (52%) of the outbreak highlights the continued need for improved research and treatment strategies to improve outcomes in infected individuals. In an excerpt from a recent conversation with Dr. Steven Bradfute, an Ebola expert who has worked at The United States Army Medical Research Institute of Infectious Diseases (USAMRIID) in Fort Detrick, Md., he explained recent developments in vaccine strategies and groundbreaking research for investigating Ebola-infection mechanisms using mice engrafted with a human immune system. Dr. Bradfute is currently focused on vaccine development for Ebola and other infectious diseases at the University of New Mexico Health Sciences Center.
The devastating mortality rate (52%) of the outbreak highlights the continued need for improved research and treatment strategies to improve outcomes in infected individuals. In an excerpt from a recent conversation with Dr. Steven Bradfute, an Ebola expert who has worked at The United States Army Medical Research Institute of Infectious Diseases (USAMRIID) in Fort Detrick, Md., he explained recent developments in vaccine strategies and groundbreaking research for investigating Ebola-infection mechanisms using mice engrafted with a human immune system. Dr. Bradfute is currently focused on vaccine development for Ebola and other infectious diseases at the University of New Mexico Health Sciences Center.
Q: What can you tell us about the latest developments in the generation of efficient vaccines for Ebola virus?
A:T here are several Ebola vaccines that are effective in non-human primate models. Although none have been tested in infected humans, some have been or are moving into Phase I clinical trials. The Ebola vaccine platforms are quite varied, ranging from virus-like particle vaccines to those based on expression of a single Ebola gene from different non-pathogenic viruses, such as replication-deficient adenovirus or live vesicular stomatitis virus. There has been some discussion on using experimental Ebola vaccines in the current outbreak, but it’s too soon to tell whether this will occur. My work focuses on improving immunogenicity to Ebola proteins regardless of the vaccine platform used.
Q: What does it take to work with the wild-type Ebola virus in a research lab?
A: We can do fascinating studies to understand how Ebola works, although it is cumbersome work. There are only a few biosafety level 4 (BSL4) facilities in the country that are designed to work safely with the wild type Ebola virus. Initially you need to go through about a year of training to work with the virus in a BSL4 laboratory. Due to these and other security measures, there has never been an environmental release from a BSL4 facility in North America .
Q: What kinds of mouse models did you use at USAMRIID?
A: We know that in patients, Ebola virus can infect macrophages and replicate inside these cells. It then gets distributed to other cells and tissues around the body, including other key players in the immune system. When the body’s early response is blocked, the virus can replicate more easily.
In collaboration with JAX Professor Dr. Lenny Shultz and University of Massachusetts Professor Dr. Dale Greiner, we used humanized NSG mice engrafted with human CD34+ hematopoietic cells (that eventually produce several types of circulating human immune cell types). We were able to verify that Ebola virus is not only detected in human macrophages, but it actively replicates inside them.
In another set of experiments we used a handy little model consisting of humanized NSG mice engrafted with human PBMCs, showing that when these mice are infected with the mouse-adapted Ebola virus, circulating human immune cells elicited a significant response by producing human cytokines, followed by induced apoptotic human T cell death. Early results suggest this model recapitulates the cytokine storm often seen in patients, sending other branches of the immune response into overdrive, often resulting in mortality.”
Q: Are humanized NSG models also helpful for developing better vaccines for Ebola?
A: There are several efficacious vaccines for viral pathogens; however, for several of them, no one knows how they work. Although I have not used this model for vaccine development yet, humanized mice are a good platform to look at how vaccines can target individual populations of immune components. You can use this model to learn more about how effective vaccines actually work. Humanized mice can be used to track where the vaccine traffics and how they activate different immune subtypes. One could also infect these mice and look for different treatments to try to decrease the viral burden in specific cell types.
Until the most recent Ebola outbreak, the pharmaceutical industry showed little interest in developing an effective vaccine to this virus. One reason for this is because in the wide spectrum of human diseases, Ebola only affects a small percentage of people who typically live in remote areas. We are grateful to the academic and government researchers around the world who persist in their quest to understand and prevent Ebola disease, even if this happens in places so far away from home.