Many of us use wearable devices and health trackers, but how can this collected data be used to keep us healthy and disease free?
Like one in five Americans, I wear a watch that also tracks several health-related statistics through the day. It tells me how well I slept, how many steps I took, how high my heart rate got during a workout, and more. While it’s not 100% accurate all the time, it’s pretty close. And if one pays any attention at all, patterns become quite apparent after months and years of use. Admittedly it tells me many things I already know—yes, it was a hard workout today; no, I didn’t sleep as long or well as I wanted to—but I still find it fun to put numbers on them. And at times it reveals far less obvious traits. For example, I’ve noticed that my resting heart rate will rise a day or two before I show symptoms of being ill.
And while much of one’s own wearable information may be obvious, that of a large population is not. So if those data points are pooled in aggregate from many wearable users, that information has a lot of potential clinical benefit. The continual data gathering of such devices reveals baselines and patterns that even regular clinical measurements are unable to detect. So it’s no surprise that the National Institutes of Health (NIH) teamed up with Fitbit in 2019 to collect participant data—namely physical activity, heart rate and sleep patterns—as part of its All of Us precision medicine research program. And Apple and Stanford collaborated for the Apple Heart Study, in which Apple Watch users provided data to provide insight into cardiovascular function and disease.
Such studies can be set up carefully and identify motivated cohorts, however. With the onset of the COVID-19 pandemic in early 2020, there was—and still remains—an acute need to track viral spread, patient response and post-infection recovery quickly, and on a large scale. Could wearable data also provide helpful, real-time information during such a crisis?
My Data Helps
A team from Scripps research noted early in the pandemic that the most common methods used to detect infection—questions about symptoms and temperature measurements—failed to detect a high percentage of cases. Indeed, research has shown that only 12% of people who tested positive for COVID-19 had a temperature above 100 degrees F. They therefore launched an app-based research platform called DETECT (Digital Engagement and Tracking for Early Control and Treatment). The goal was to determine if combining changes in sensor data with symptom data could be used to improve the ability to detect COVID-19 positive individuals who self-reported symptoms.
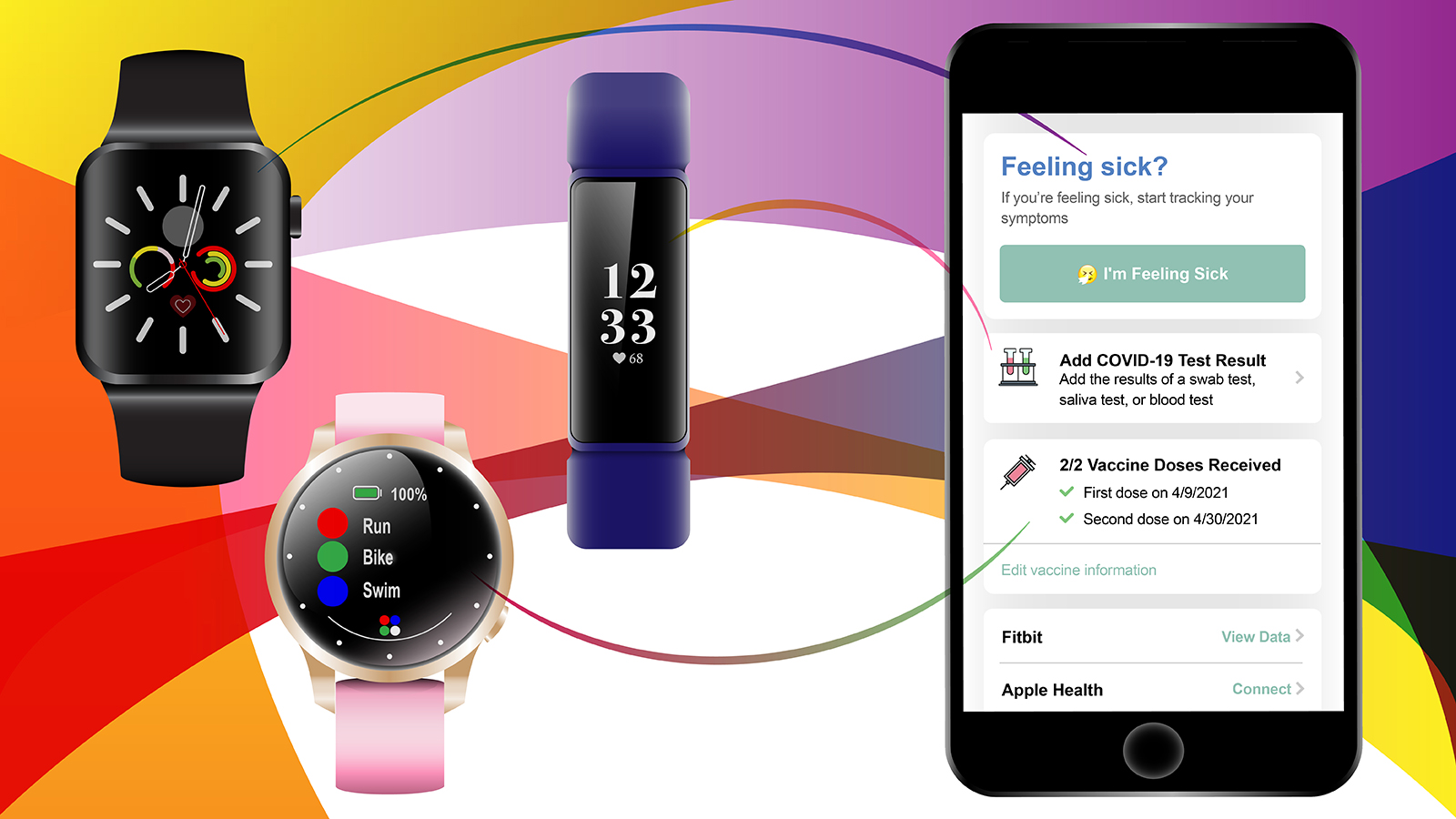
As reported in a paper published in Nature Medicine, the study rapidly enrolled more than 30,000 people between March and June 2020 (including me), who shared data from Fitbit, Apple and Google devices. The device connection provided sleep data, resting heart rate and activity levels. Through a smartphone app, called MyDataHelps, participants also self-reported any illness and symptoms, as well as COVID-19 test results and vaccination date(s). The authors analyzed the data from 54 people in the study group who reported COVID-19 infections, and they compared the ability to distinguish between them and 279 COVID-negative controls.
What they found was that using the full set of wearable data alone was as effective as symptom self-reporting, but combining the two provided far better distinction between the two groups than either method alone. The study was relatively small, but it provided an encouraging look at the power of wearable data. Its conclusions were also similar to a separate study with slightly different methodology completed by Michael Snyder’s group at Stanford, which has long investigated the clinical utility of “baseline” data from wearable technology. While there are obvious limitations involved, starting with the four out of five Americans who do not own or use a wearable health or fitness tracker, wearable technology is already providing deeper, more consistent data than can be obtained through occasional clinical visits. And that data has the potential to be valuable during a health crisis.
The long COVID road
Another aspect of wearable data is that it is longitudinal, consistently collected over long periods of time. This is a key attribute for another troubling aspect of the COVID-19 pandemic—for some people, the symptoms and debility drag on and on. So-called “long COVID” is mysterious, as its underlying cause(s) remain unknown, and it’s unpredictable, afflicting some people who had mild or even asymptomatic disease and not others who had severe cases. Scripps researchers therefore leveraged the DETECT data collection, which is ongoing and growing (now at 37,000 people reporting data), to track those who had COVID-19 infections in the weeks and months after their positive tests and see what their data showed.
Out of 875 study participants that had reported symptoms of a respiratory illness (e.g., coughing, body aches), 234 ultimately tested positive for COVID-19. All of them slept more and walked/moved less after they got sick, but those with COVID-19 showed far great relative changes. Even more striking was the change in resting heart rates, which also rose in everyone but returned to normal in just four days in those in the non-COVID group. For those with COVID-19, the elevated heart rate persisted for weeks, then months. The average time it took to return to normal was 79 days and for some it took more than four months, underscoring the stark differences between COVID-19 and other respiratory infections. It may even indicate that COVID affects the autonomic nervous system, which regulates heart rate.
The study is preliminary, but it has opened the door to future research and the data collected is already providing clues to what long COVID actually is and how it affects the body. Also, the NIH is now providing $1.15 billion to fund research into long COVID, much of which may lean on wearables for long-term data collection. It can be hoped that the insight gained will mean an end to the COVID-19 pandemic for everyone, without post-infection illness and disability stretching into the future.