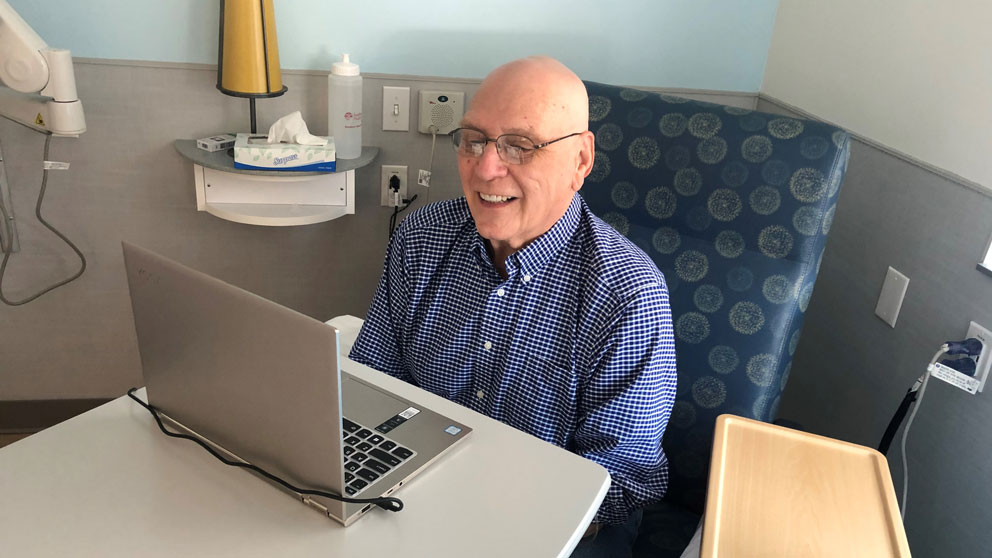
John Pierce is a cancer patient who is participating in the Maine Cancer Genomics Initiative. Pierce was able to take part in the MCGI tumor board meeting online in March. Photo by Alexandra Giardino.
From cancer genomic testing to clinical trials, John Pierce is exploring the latest advances to address his medical issues.
What advice would John Pierce give to someone who has just received a cancer diagnosis? “First, be your own best advocate. When I was a 20-year-old combat helicopter pilot in Vietnam, I learned that when someone or something is trying to kill you every day, you recognize that nothing focuses your mind like your own mortality.”
Second, he says, “get genomic profiling.”
Nearly 50 years after his combat experience, Pierce is now retired from a successful and varied career as an internet consultant. And following a series of unusual health crises that trained him to seek out the best medical advice and treatment, he has been diagnosed with cholangiocarcinoma — a very rare cancer of the bile ducts, the slender tubes that carry the digestive fluid bile through the liver. Pierce is now bringing his lifelong facility for quickly acquiring technical expertise to his treatment regime, to be his own best advocate.
Pierce may not be your average cancer patient, but every patient, and every cancer, is genomically unique. Pierce says that when he learned he had cancer, “my first inclination was to obtain genomic testing. Cancer isn’t liver cancer or lung cancer; it’s defined by whatever the cancer’s genomic profile is. And that’s why I started down this path and requested testing.”
Pierce’s oncologist is Roger Inhorn, M.D., Ph.D., of MaineHealth, a steering committee member of the Maine Cancer Genomics Initiative (MCGI). JAX founded MCGI in 2016 with a grant from the Harold Alfond™ Foundation and has enrolled every oncology practice in Maine and most of its oncologists. In phase one of the program, which concluded at the end of 2020, participating oncologists submitted patient tumor samples to be sequenced and profiled for genes known to be associated with various cancers, and with response or resistance to approved targeted therapies or new drugs in development approved by the U.S. Food and Drug Administration.
“For almost all of my patients who have an advanced malignancy and have enough tissue available,” Inhorn says, “I offered participation in MCGI. Genomic profile testing helps clarify potential options by looking for targetable mutations for which there might be either a clinical trial option or a commercially available drug that can be used to treat their malignancy.”
Inhorn notes that like many patients participating in MCGI, Pierce “understands that there is also an altruistic piece to this. They understand that MCGI and the clinical community are trying to learn and create a larger database of treatment options and to engage and educate oncologists about how to best use these platforms. I think the day is coming where everyone who has an advanced malignancy will be offered genomic profiling — it’s going to become a standard of care.”
Tumor profiles from MCGI testing, and their best treatment options, are reviewed at Genomic Tumor Board (GTB) sessions, virtual conferences that link clinicians with experts in cancer genomics and clinical trials. Inhorn mentioned to Pierce that there was a tumor board meeting coming up, and Pierce said, “I’d like to participate. I’d like to be in the room when they’re discussing my case.”
Jens Rueter, M.D., medical director of MCGI, says that Pierce’s participation in the tumor board “worked out really well. Beforehand I was a little bit nervous about it because I didn’t really know what to expect. He’s an unusual individual because he embraces new technologies, and that’s coupled with really wanting to impact his treatment plan dramatically.”
Rueter says GTBs are an important component of MCGI, as they often provide the most significant input to clinicians with respect to applying the genomic information in their patients’ care plan. Typically, four cases are discussed during each one‑hour meeting. A brief case presentation by the treating oncologist is followed by a presentation of the genomic case information. Then, external advisors specializing in precision oncology give their interpretation of the case and provide significant guidance to the oncologist and the medical team. In this case Pierce himself was also able to query the experts.
Genomic testing identified two targetable mutations in Pierce’s cancer. He is now on his second targeted therapy (erlotinib) after four months on the IDH2 inhibitor enasidenib.
According to Rueter, most cancer patients fall into one of two categories. “The first are comfortable doing what their doctor says, maybe asking questions or even questioning some decisions, but basically trusting the doctor. And the second tend to shop around for doctors until they find the one who tells them what they want to hear.” Pierce is in a rare third category, Rueter says. “He just wants to know everything that could possibly be done to address his cancer.”
Pierce is continuing to actively advocate for his health. “I think cancer and oncology clinicians today don’t talk about cures; they talk about control. And as far as I’m concerned, control isn’t really good enough for what I’m looking for. I am looking for a cure.”
MCGI The Maine Cancer Genomics Initiative
The Maine Cancer Genomics Initiative (MCGI), a collaboration aimed at making the latest personalized medicine available to cancer patients throughout Maine, will now bring new precision oncology clinical trials to the state, support access to targeted therapies for patients not eligible for trials, and develop novel technology to enhance genomic education and genetic services through online platforms.
A model for personalized cancer care in a rural setting
MCGI is a statewide collaboration of JAX scientists and community oncologists that brings innovative cancer genomic testing, education and drug access infrastructure to Maine. Every oncology practice in the state is a partner in the program. Initially driven by the need for greater availability of cancer genomic testing in Maine, MCGI has become a model for community precision oncology, or personalized cancer care, in a rural setting. Precision oncology uses analysis of a patient’s normal genetics and the specific mutations found in his or her tumors to guide more targeted treatments.
“Over the last four years, we’ve made great progress with precision medicine in Maine, especially in rural areas of the state,” said MCGI Medical Director Jens Rueter, M.D. “In the first phase of the initiative, we provided genomic tests to over 1,600 cancer patients, affecting patient lives from Caribou to Kittery. Over the next five years, we will focus our efforts on helping patients navigate the steps of entering genome-informed clinical trials and of accessing targeted therapies as part of their routine medical care.”
The initiative also plans to expand its reach to other areas of the Northeast beyond Maine.
Please help us continue changing the lives of patients by providing access to cutting-edge cancer diagnostics and treatments.
we can make a difference in the lives of Maine cancer patients.